The Hidden Damage of Dry Mouth: How Xerostomia Wears Down Your Oral Environment
Share
Quick takeaways
-
Saliva is protective: It buffers acids, delivers calcium/phosphate for remineralization, washes away food/bugs, and keeps tissues comfortable.
-
Low saliva = higher acid time: pH dips last longer after eating/drinking, tipping the balance toward demineralization, decay, and erosion.
-
The ecology shifts: Sticky, acid-loving bacteria thrive; plaque hardens faster; gums get inflamed more easily.
-
Soft tissues suffer: Burning, sores, fungal overgrowth (thrush), cracked corners of the mouth, and trouble speaking/swallowing are common.
What saliva normally does (and why losing it hurts)
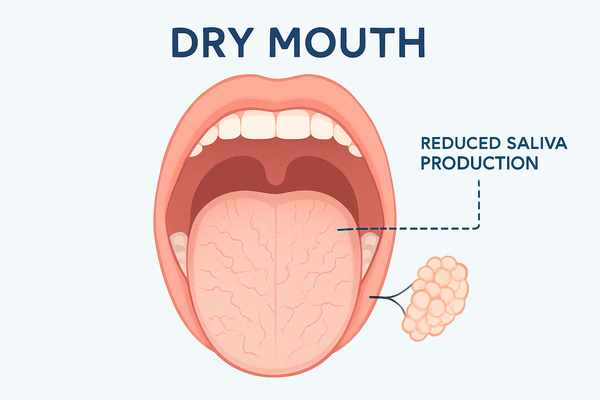
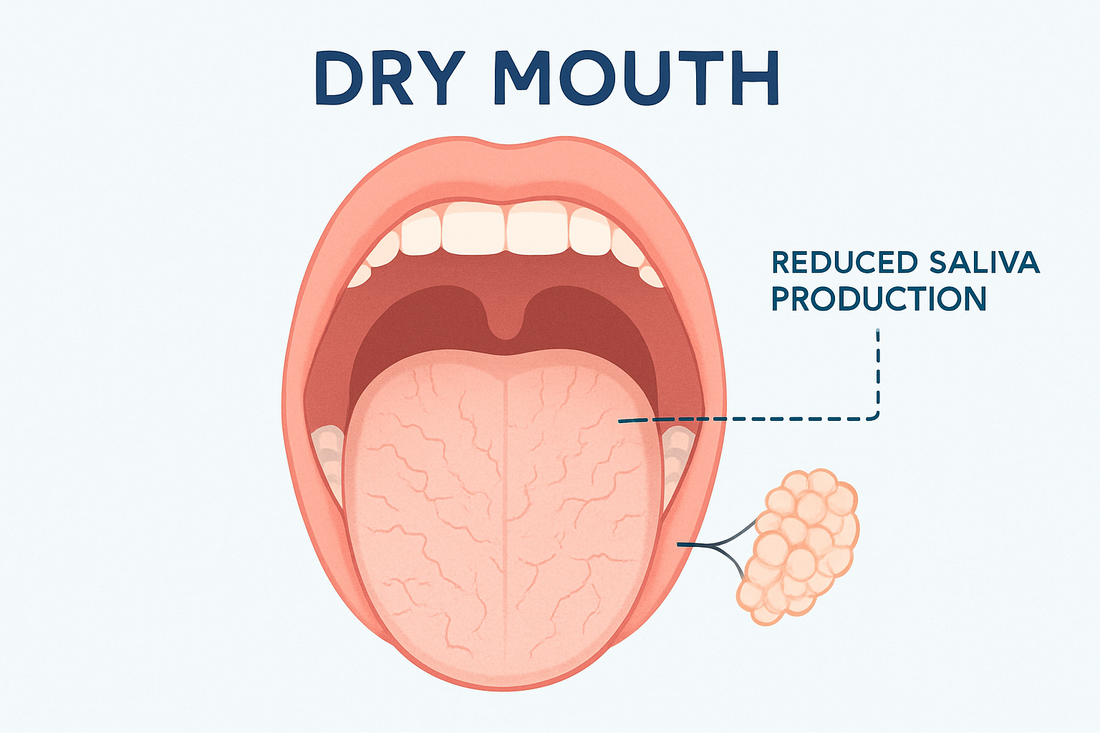
One of the first things dental students learn about the mouth and oral environment is how important saliva is for maintaining the teeth and gum tissues. When discussing this with my patients, I tell them to think of saliva as your mouth’s built in defense system. Saliva does many things, it buffers and dilutes acid, helps remineralize enamel, mechanically cleans the teeth and gums, gives antimicrobial support, and lubricates for comfort.
Buffering and diluting acid is important because acid is the main cause of cavities in the mouth. Bicarbonate and other buffers neutralize acid from food and bacterial metabolism. Less saliva = longer “acid attack”.
Saliva also helps to remineralize enamel by carrying calcium and phosphate that patch early enamel decalcifications which leads to cavities. With little saliva, the balance shifts towards a loss in minerals over time leading to decay. This happens especially on the root surfaces and along the gumline.
When a reduction in saliva occurs, mechanical cleansing also becomes diminished. A healthy flow of saliva physically washes away, sugars, acid, and free-floating bacteria. In a dry mouth, plaque accumulates faster and hardens into tarter sooner. The bacteria that accumulate in an on the tarter fuels decay and bad breathe (halitosis)
Another important note on saliva is the ability to lubricate the oral tissues. Saliva cushions and hydrates the mouth aiding in speech, swallowing, taste, and comfort. When it is scarce, tissues become fragile and inflamed which can lead to sore and sticky mucosa.
The cascade of damage when you’re dry
Cavities (especially root & cervical caries)
When the buffering ability of the saliva is reduced, decay happens at a much faster rate due to the body’s natural defense mechanism not working to its full potential. This tooth structure breakdown is more likely to occur at the gumline and along the root surfaces (exposed by recession) due to the lack of enamel in these areas. No enamel = less protection.
Enamel erosion & tooth wear
Without saliva’s buffering, dietary acids (sodas, citrus, sports drinks) and gastric reflux do more harm. The teeth may begin to look yellowed (dentin showing), feel sensitive, and show cupping or flattened facets.
Gum inflammation & faster tartar build-up
Lack of saliva leads to sticky plaque which is harder to clear when your mouth is dry. More plaque, more gingival inflammation and bleeding due to biofilm and bacterial buildup. When saliva is mineral-rich but stagnant, faster calculus (tartar) formation occurs, locking in the cycle.
Bad breath (halitosis) and taste changes
Dry surfaces encourage sulfur-producing bacteria on the tongue and between teeth. The sulfur compounds are what causes the bad breath smell. Many patients report a metallic taste or blunted flavors when eating.
Soft-tissue problems
When the soft tissues in the mouth get dry, they have a tendency to stick together. This often creates friction and can lead to a “click” when the person talks. The friction or rubbing can lead to sores on the tongue and movable tissue in the mouth. The dryness of the tissue can also lead to:
-
Burning Mouth Syndrome
-
Recurrent ulcers
-
Candidiasis (thrush) - fungal infection
-
Daily life interferences - speaking, swallowing, talking during long conversations
Where a dry-mouth pouch can fit
A discreet, stationary pouch can deliver slow, steady relief without chewing or spraying, and can carry xylitol and citric acid (flow support), hyaluronic acid (tissue hydration), and nHA (enamel support) while buffering acids. Many people use a pouch during meetings, travel, and long calls, then switch to a nighttime strategy.
Bottom line
Dry mouth isn’t just a nuisance—it reshapes your oral ecosystem. Protecting yourself means restoring the balance: stabilize pH, support remineralization, and keep tissues comfortable. With smart daily habits, the right at-home products, and professional guidance, you can slow or even reverse much of the damage.